Root Canal Therapy
Best approach when deciding if you should have root canal therapy and when to address teeth that have been previously treated
S. WARD ECCLES, D.D.S.
Welcome New Patients
About Us
Root Canal Therapy

What is root canal therapy
Diagnosing Treatment
It’s important to use diagnostic imaging and techniques to insure the condition of the tooth as well as the right option to treat the tooth.
When not to treat
You should not consider root canal therapy when the root is cracked or the tooth is too disruptive to your body’s overall health.
Treating Infected Teeth
Root Canal Filling Material
We have been using heavy calcium oxide as in Endocal 10 for over 20 years, a very effective in treating infected root canals
Restoring Tooth After Treatment
What is Root Canal Therapy
Some say that all “dead teeth” are bad. It is bad to keep a treated or untreated dead tooth in your mouth that is still infecting your body 24 hours a day. Bacteria, their toxins, and the inflammation products spread from dentinal tubules to the surrounding bone and into the bloodstream to the rest of the body. This is what occurs with traditional gutta percha filling material. It is true that with only the main canal(s) filled; most pain and swelling does subside.
Diagnosing the Need for Treatment

It’s important to use diagnostic imaging and techniques to insure the condition of the tooth as well as the right option to treat the tooth.
Radiograph: an x-ray can show infection in the apex of the tooth. Where there may be unusual shapes and extensions of canal anatomy, a CBCT (3-D scan) may be recommended. Some infections may not be detected on x-rays.
Vitality Test: Electrical or temperature to test the response or lack of response from stimulating the nerve inside the tooth from the surface.
Muscle Testing: Applied kinesiology using the body’s energy reflex and acupuncture meridians to determine if a tooth may be causing dysfunctions within the body.
Review of current medical conditions: A review of current medical and health conditions as well as lifestyle preferences is done to ensure saving a sick tooth with a root canal is the right course of action. For some patients with major health conditions, it may be best to extract the sick tooth.
What remains unstopped is exposure to toxins produced from bacteria still living in the thousands of tiny pore (dentinal tubules) openings that reach from the root surface to the center of the tooth. These pores are too small to access and get into to be cleaned. Lasers may clean in a straight line within the canal. However, only the opening of the tubules that extend to the root surface within a straight line or 90 degree offshoots, but no further. This means the tissue and bone anchoring the root are still chronically infected from these tubules even after “successful” treatment of the root canal.
When Not To Treat

You should not consider root canal therapy for:
- Cracked root – just because a tooth is cracked, it does not warrant the need for root canal treatment. Only if the nerve itself is inflamed (and cannot be resolved) or the tooth starts to bleed.
- Medical practitioner (including naturopaths or functional medicine practitioners ) finds tooth too disruptive to your body’s overall health
- You simply would rather have it removed and rid yourself of the tooth (always better than keeping an untreated or treated, infected tooth)
- Sensitivity to all types of root canal filling materials
The standard criteria for successful root canal treatment is:
- It stopped hurting
- X-ray shows healing of infection
Health centered or biological dentistry goes one step further:
No remaining bacteria/toxins in tubules that continuously leak to the body and overwork an already busy immune system.
Alternative Treatment:
If it has been determined that the tooth is negatively affecting the body without a good prognosis, it may be healthier for the body to extract the tooth. There are options to replace an extracted tooth including removable appliance, fixed bridge, and nonmetal implants.
Treating Infected and Dead Teeth
Antibiotics:
It is common for endodontists ‘root canal specialists” to prescribe antibiotics and pain meds for patients receiving root canal treatment. I rarely prescribe antibiotics nor pain medication as it is only needed if there is already swelling in the surrounding tissues. Swelling around the tooth can also be addressed using gaseous oxygen-ozone via injection around the tooth or by opening an access hole in the tooth to relieve the pressure and commence root canal treatment.
Pulp Regeneration:
On a vital tooth where the pulp may be exposed, a pulp cap can be done and the tooth will be monitored over the following 1-6 months. Many times root canal therapy can be avoided by treating the exposed (or almost) pulp tissue by
- thoroughly cleaning the expose pulp
- sterilizing the remaining pulp tissue with oxygen-ozone (Sterilizing is KEY to allow it to heal)
- Capping the perforation to the pulp with growth stimulating minerals to encourage growth of new tooth structure
- Placing permanent or temporary restoration on the tooth to restore function.
If discomfort persists, then root canal therapy may need to be done.
Root Canal Therapy
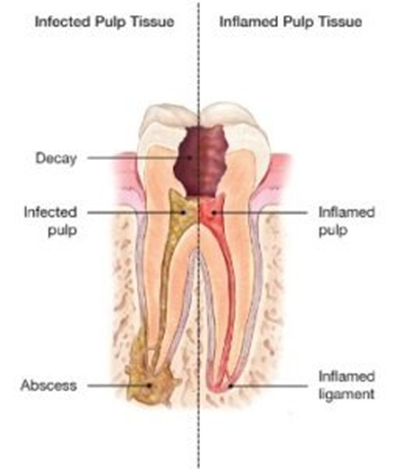
Inflamed or infected teeth are the most common reason for root canal therapy. This can be caused by deep decay, repeated dental procedures on the tooth, or accident/damage to the tooth. If pulp inflammation or infection is left untreated, it can cause pain, lingering sensitivity to hot or cold, and/or lead to an abscess.
- A digital x-ray may show the extent of the decay or abscess. It may be necessary to take one to fully diagnose.
- For your protection, a small protective sheet or “dental dam” is placed over the tooth to isolate and keep the area free of saliva during the procedure.
- A small hole is made in the tooth to access the inside of the tooth
- Dental files are used to remove pulp tissue and shape the canals to a point at the end of the tooth (apex).
- Continuous irrigation with ozonated water kills all bacteria inside the tooth (especially accessory canals). We never use chlorine bleach
- Some teeth have additional canals that may need to be treated at a subquencial visit.
- When a tooth is left untreated, calcification within the canals can occur. This creates blockages that are hard to remove and may require more time or visits.
- Once the inside of the tooth has been filed and cleaned, the tooth must be filled or sealed from the inside.
Re-treatment
The most common reason a tooth needs to be retreated is the return of bacteria inside the tooth. Because teeth have accessory canals or “dentinal tubules” bacteria can seep inside of the tooth.. This lingering bacteria can reinfect the tooth, especially if the seal is defective. However, retreatment can be the best option for some patients.
Retreatments are a labor intensive procedure. It includes:
- Tedious dissection and removal of pre-existing root canal filling material
- Removal of metal posts, if placed
- Removing additional calcified blackages
- Goes through the same irrigation and sterilization process
Root Canal Filling Material – EndoCal 10 (DISCOUNTINUED)
In order to complete root canal therapy, the canals must be cleaned, sterilized and filled.
- I have been using heavy calcium oxide as in Endocal 10 for over 20 years. I have found it very effective and successful in treating infected root canals. I mix it with Yttrium oxide to show up better in an x-ray and also a probiotic powder to improve the environment inside the tooth.
- There was a study with 15 extracted teeth using Endocal 10. 3 of them resulted in cracked teeth. I never see this with teeth still in the mouth. Root canal specialists love to quote this study without finding out for themselves how effective this treatment really is. Some claim the material expands to crack the teeth – not so. There is no expansion in volume. It expands linearly – or is drawn toward moisture and “wicks” into the small tubules in the roots and fills and seals them. This is a very positive characteristic. It is also drawn by moisture to infection in the bone around the root where its alkaline properties help neutralize the infection and quickly restore comfort.
- If there are no pre-existing cracks (Note: there can be hairline cracks not visible at first. Many teeth that have or previously had mercury amalgam fillings, have vertical and horizontal cracks. This results from the metal filling expanding.) These cracks, if extending down into the root, will cause the root canal therapy to fail. The moisture in the cracks will draw in the paste filling material by “wicking” or capillary action. This paste is very beneficial in non-cracked teeth as it is drawn into the microscope dentine tubules to neutralize the bacteria that are there.

- Again, the paste does not expand by volume, but moves linearly. Once in the tubules it sets up and seals the tubules. If it can be predetermined that cracks are present that extend to the roots, then root canal therapy will not be started or at least you will be informed of a decreased chance of successful treatment. You can then weigh the risk involved before proceeding. No matter what root canal filling material is used, if there are vertical cracks extending to the roots, it is a matter of time until they fail.
- Fill with Endocal 10, which is heavy calcium oxide. This wet paste is drawn into the tubules before it hardens from the main canal by “wicking” as in a kerosene lamp. This results in a very clean tooth then filled quite thoroughly both vertically and horizontally. This isn’t a perfect tooth but has the best chance to not contribute to the downfall of your teeth.
Restoring a Tooth after Root Canal Treatment
Once a tooth has received root canal therapy it will need a restoration. If the tooth is not restored, it leaves it weak and susceptible to breaking. The type of needed restoration depends how much tooth structure has to be removed and how much is remaining.
Strategies for Biocompatible Endodontics
Filling: If a small amount of tooth structure was removed during the root canal process, a resin composite dental filling can be done to restore the tooth’s structure.
Build Up: If deep decay is present, a build up is needed to fill in the hollowed out tooth’s crown “top of tooth”.
Post: Previously it was taught the metal posts were needed after all root canal fillings. It was found that a flexing tooth with a non-flexing post resulted in cracked teeth. It was later determined that a post was seldom needed where there was sufficient tooth structure remaining to support a reinforcing build-up prior to crown replacement. When a post is required, they are now made of non-metal and similar physical properties to tooth structure.
Crown: If a majority of the tooth structure is gone, a crown will be needed to replace the full function of the tooth.
Biological Dentistry
Using science-based, biological techniques, technologies, and materials for your oral and overall health
Family Dentistry
Establishing preventative dental care routine and restorative treatment options for the entire family
Safe Mercury Removal
Replacing amalgams with non-toxic filling materials while safely capturing released mercury
Root Canal
Emphasizing a biological approach to diagnosing and treating infected teeth
Gum Therapy
Addressing periodontal “gum” disease systemically and non-surgically
Cosmetic Dentistry
Restoring and replacing natural teeth using a conservative approach with non-metal materials
Dental Surgery
Our dental surgery approach respects the body’s natural ability to heal
TMJ Therapy
TMJ dysfunction causes jaw pain, facial tension, headaches & neck discomfort
Ozone Therapy
A safe, natural treatment to disinfect & reduce inflammation

